"Family-centered" nursing model to help extremely premature babies gain a new life!
Family-centered care model
"Family-centered care" (FCC) is a new nursing model favored by developed countries. Its core concepts are to respect children and families, transmit health information, respect family members' choice, emphasize cooperation among children, families and caregivers, and give strength and support. The concept was proposed in the United States as early as 1972, and in recent years it has been widely carried out in Canada, Finland and Australia. In China, due to the medical environment, shortage of nursing staff, family concept and other reasons, the whole line is limited. FCC is a nursing model based on integration, personalization and establishment of doctor-patient cooperation, which fits the patient-centered management philosophy of our hospital. FCC project in neonatology department not only conforms to the cultural requirements of the hospital, but also the development trend of NICU nursing.
The baby was born 29+4 weeks preterm with a birth weight of 1.05kg and dyspnea at birth. Consider neonatal respiratory distress syndrome, very premature infants, very low birth weight infants, immediately after delivery of respiratory support transferred to the neonatal NICU for further treatment.
The treatment process of very premature infants is complicated, difficult, time-consuming and costly, and prone to various complications such as infection, intracranial hemorrhage, gastrointestinal hemorrhage and necrosis, chronic lung disease, etc., which increases the difficulty of treatment and the length of hospitalization, and even endangers life, requiring extremely high medical treatment and nursing.

In the face of various difficulties and family economic difficulties, the family was full of confusion and hesitation, and once wanted to give up. Medical staff in the department should discuss cases in time and formulate diagnosis and treatment plans. In order to achieve better treatment results, the neonatal department decided to apply FCC protocol to this child.
Wu Qianqian, attending physician of neonatology department, was in charge of the whole diagnosis and treatment of children, and the department gave full support and cooperation. Dr. Wu immediately went to the obstetrics department to further understand the family situation of the child and communicate with the family in depth. Carefully and patiently analyze the condition and possible prognosis of the children, and inform the department's diagnosis and treatment plan and the benefits of FCC in detail. After answering questions, the family understood the strength of the neonatology department and the advanced treatment and nursing mode.
The medical staff will invite the baby's parents into the ward to participate in the care. It will feed the baby as soon as possible, and it is breast milk, and it will switch to total intestinal nutrition as soon as possible, reduce injections, reduce intravenous nutrition days, promote defecation and reduce enema and other invasive operations, which can improve lung ventilation, help establish rules for autonomous breathing, reduce ventilator dependence, get off the ventilator as soon as possible, reduce hospital days and costs. At the same time, parents not only have skin contact and family companionship with their babies during their stay in the ward, but also learn nursing and first-aid knowledge. In the long run, it can improve lung development, promote brain development and reduce brain sequelae. The big stone in the heart of the family was finally put down, and the whole family was confident, gladly accepted the treatment, and said that they would do their best to save the children.
This is the first FCC operation project in Zhangzhou City. Director Huang Zhongling, the discipline leader, attaches great importance to the introduction of new international ideas and new progress, and arranged for attending physician Wu Qianqian to study the FCC project in Shenzhen Hospital of the University of Hong Kong for half a year last year to prepare for this operation. With the encouragement of Dr. Wu, Bao Ma sent colostrum 14 hours after birth and applied it to the mouth for colostrum oral immunotherapy. At 17 hours after birth, the child was opened to breastfeed exclusively. Total enteral nutrition was achieved 12 days after birth, with a weight of 1.46kg and no more injections and transfusions.
On the fifth day after birth, Bao Ma officially entered the NICU and integrated into the family nursing. Through kangaroo care to establish skin-to-skin contact and transfer family affection, the baby is quiet and satisfied in the mother's arms, breathing smoothly, breast milk digestion is good, the mother often participates in nasal feeding, sucking training, changing diapers, wiping bath and other daily care, baby mother to establish a good parent-child relationship, Mother from the nervous, nervous to gradually establish a mutual assistance partnership with the medical staff, talk about baby care, talk about home affairs, the mother is happy, postpartum recovery is good, the family is taking care of the treasure mother every day, escorting the treasure mother into the ward on time, family relations become harmonious and warm.
- ABB
- General Electric
- EMERSON
- Honeywell
- HIMA
- ALSTOM
- Rolls-Royce
- MOTOROLA
- Rockwell
- Siemens
- Woodward
- YOKOGAWA
- FOXBORO
- KOLLMORGEN
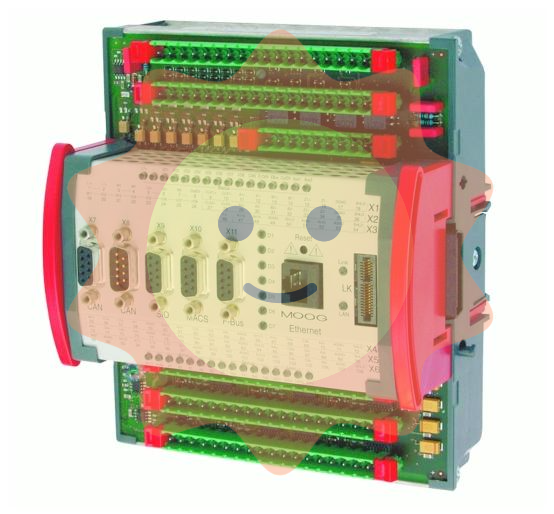
- MOOG
- KB
- YAMAHA
- BENDER
- TEKTRONIX
- Westinghouse
- AMAT
- AB
- XYCOM
- Yaskawa
- B&R
- Schneider
- Kongsberg
- NI
- WATLOW
- ProSoft
- SEW
- ADVANCED
- Reliance
- TRICONEX
- METSO
- MAN
- Advantest
- STUDER
- KONGSBERG
- DANAHER MOTION
- Bently
- Galil
- EATON
- MOLEX
- DEIF
- B&W
- ZYGO
- Aerotech
- DANFOSS
- Beijer
- Moxa
- Rexroth
- Johnson
- WAGO
- TOSHIBA
- BMCM
- SMC
- HITACHI
- HIRSCHMANN
- Application field
- XP POWER
- CTI
- TRICON
- STOBER
- Thinklogical
- Horner Automation
- Meggitt
- Fanuc
- Baldor
- SHINKAWA
- Other Brands